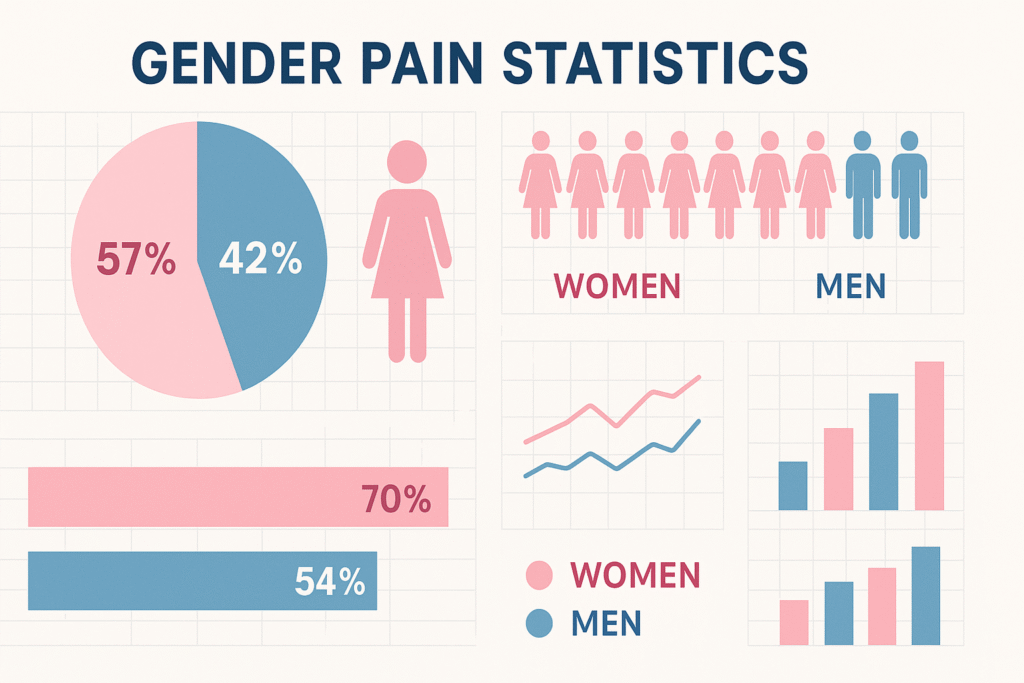
Chronic pain affects millions of people worldwide, but the burden isn’t equally distributed. Research consistently shows that women experience chronic pain more frequently, more intensely, and for longer durations than men. Despite representing 70% of chronic pain sufferers, women face significant disparities in both pain research and treatment approaches. Understanding these gender differences is crucial for improving pain management and achieving healthcare equity.
The Stark Reality: Women and Chronic Pain Statistics
The numbers paint a clear picture of gender disparities in chronic pain:
- 70% of chronic pain sufferers are women, yet 80% of pain studies are conducted on male subjects
- Women are 7 times more likely to be misdiagnosed during heart attacks due to pain presentation differences
- In emergency rooms, women wait an average of 65 minutes for pain relief compared to 49 minutes for men
- Women are more likely to receive sedatives instead of pain medication for the same conditions
- 3-to-1 female-to-male ratio exists for irritable bowel syndrome diagnosis
- Migraine prevalence affects 18% of women versus only 7% of men
These statistics reveal not just biological differences, but systemic issues in how women’s pain is perceived, studied, and treated within healthcare systems.
Why Women Experience More Chronic Pain: The Biological Foundation
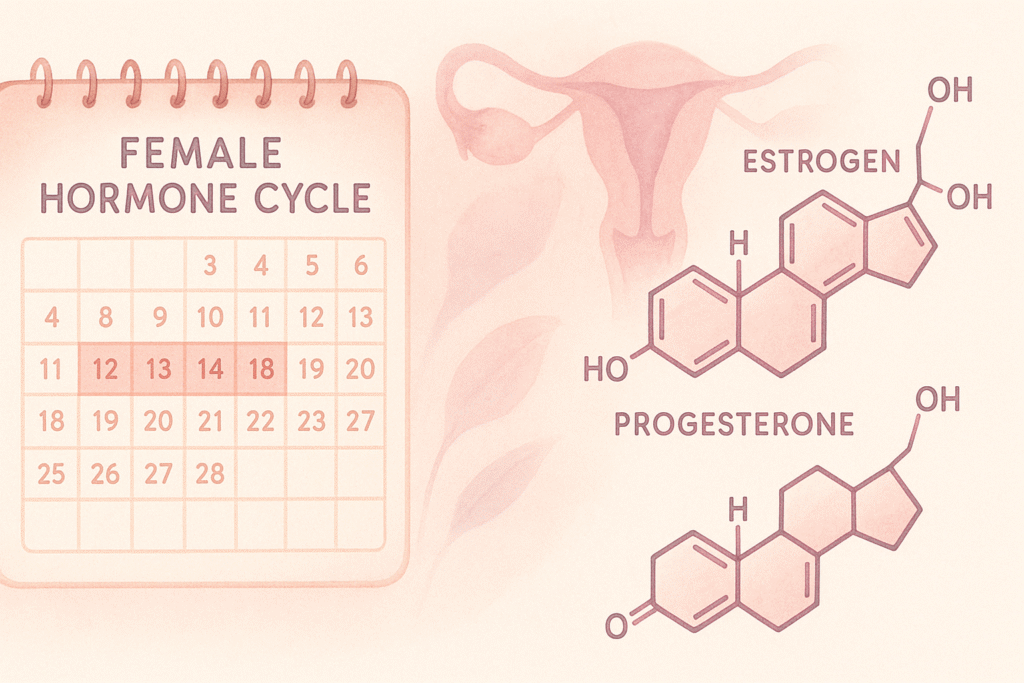
Hormonal Influences Throughout the Lifecycle
Hormones play a pivotal role in pain perception and chronic pain development. Estrogen and progesterone fluctuations throughout a woman’s life significantly impact pain sensitivity:
Menstrual Cycle Effects:
- Estrogen levels influence pain threshold and tolerance
- Pre-menstrual periods often correlate with increased pain sensitivity
- Hormonal contraceptives can either alleviate or exacerbate chronic pain conditions
Pregnancy and Postpartum:
- Relaxin hormone increases joint flexibility, potentially leading to musculoskeletal pain
- Postpartum hormonal crashes can trigger or worsen chronic pain conditions
- Pregnancy-related conditions like symphysis pubis dysfunction can develop into chronic pelvic pain
Menopause Transition:
- Declining estrogen levels correlate with increased pain sensitivity
- Bone density loss accelerates, contributing to musculoskeletal pain
- Sleep disruption from hormonal changes can worsen existing pain conditions
Neurological and Anatomical Differences
Women’s nervous systems process pain differently than men’s:
- Increased nerve density in female bodies may contribute to heightened pain sensitivity
- Brain processing differences show women activate more regions associated with emotional pain processing
- Genetic factors influence pain receptor sensitivity, with some variants more common in women
- Neurotransmitter differences affect how pain signals are modulated in the brain
Types of Chronic Pain Disproportionately Affecting Women
Musculoskeletal Pain Conditions
Research across 17 countries involving over 85,000 participants confirms that musculoskeletal pain is significantly more common in women:
Fibromyalgia:
- Affects 2-4% of the population, with 80-90% being women
- Characterized by widespread pain, fatigue, and tender points
- Often co-occurs with other conditions like irritable bowel syndrome and migraines
Rheumatoid Arthritis:
- Women are 2-3 times more likely to develop this autoimmune condition
- Hormonal factors may trigger onset, particularly during reproductive years
- Requires specialized treatment approaches considering hormonal influences
Chronic Back and Neck Pain:
- Higher prevalence in women, often related to anatomical differences
- Pregnancy and childbirth can contribute to long-term spinal issues
- Occupational factors and caregiving responsibilities may exacerbate symptoms
Abdominal and Pelvic Pain Disorders
Endometriosis:
- Affects 10-15% of reproductive-age women
- Can cause debilitating pelvic pain that significantly impacts quality of life
- Often misdiagnosed or dismissed, leading to delayed treatment
Irritable Bowel Syndrome (IBS):
- 3-to-1 female predominance
- Symptoms often fluctuate with menstrual cycles
- Requires individualized treatment approaches considering hormonal influences
Chronic Pelvic Pain:
- Can result from multiple conditions including endometriosis, pelvic inflammatory disease, or trauma
- Strong correlation with intimate partner violence (affecting 1 in 4 US women)
- Requires comprehensive, multidisciplinary treatment approaches
Headache and Migraine Disorders
Migraine Prevalence:
- Affects 18% of women compared to 7% of men
- Often triggered by hormonal fluctuations
- Women report more painful, longer-lasting episodes with additional symptoms
Tension-Type Headaches:
- More frequent in women, often stress-related
- Can evolve into chronic daily headache patterns
- Requires addressing both physical and psychological triggers
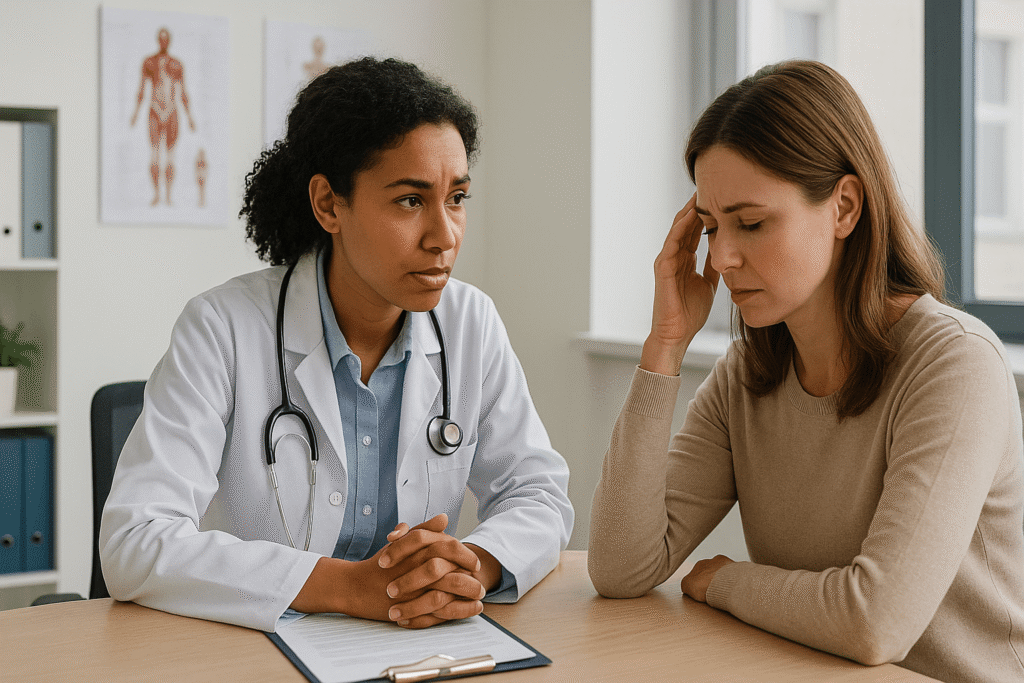
The Treatment Disparity Crisis
Medical Bias in Pain Assessment
Women face significant bias in healthcare settings when seeking pain treatment:
- Pain minimization: Women’s pain is more likely to be attributed to psychological rather than physical causes
- Delayed diagnosis: Conditions like endometriosis take an average of 7-12 years to diagnose
- Inadequate pain relief: Women receive less aggressive pain management compared to men
- Research gap: The overwhelming focus on male subjects in pain research limits treatment options
Cultural and Societal Factors
Beyond biological differences, cultural factors influence how women experience and report pain:
- Socialization differences: Women are often taught to endure pain silently
- Caregiving responsibilities: Women may delay seeking treatment due to family obligations
- Economic factors: Women may have less access to comprehensive healthcare
- Communication styles: Differences in how women describe pain may lead to misunderstanding
Comprehensive Treatment Approaches for Women’s Chronic Pain
Individualized Medical Management
Effective chronic pain treatment for women requires personalized approaches:
Hormonal Considerations:
- Timing medications with menstrual cycles
- Considering hormonal contraceptives’ impact on pain conditions
- Hormone replacement therapy evaluation during menopause
Medication Strategies:
- Gender-specific dosing considerations
- Addressing medication interactions with hormonal treatments
- Considering pregnancy and breastfeeding implications
Integrative Treatment Modalities
Physical Therapies:
- Pelvic floor physical therapy for pelvic pain conditions
- Specialized women’s health physical therapy programs
- Low-impact exercise programs designed for chronic pain management
Psychological Support:
- Cognitive behavioral therapy specifically adapted for chronic pain
- Trauma-informed care for pain conditions related to abuse or violence
- Support groups focused on women’s chronic pain experiences
Alternative Approaches:
- Acupuncture with consideration for menstrual cycle timing
- Mindfulness and meditation practices
- Nutritional interventions addressing hormonal balance
Advocating for Better Pain Care
Self-Advocacy Strategies
Women can take steps to ensure they receive appropriate pain care:
- Document symptoms: Keep detailed pain diaries including menstrual cycle correlations
- Prepare for appointments: Bring specific examples and impact statements
- Seek second opinions: Don’t accept dismissive responses to persistent pain
- Request referrals: Ask for specialists familiar with women’s pain conditions
Healthcare System Changes
Systemic improvements needed include:
- Increased research funding for women’s pain conditions
- Gender-inclusive pain research protocols
- Provider education on gender differences in pain
- Standardized assessment tools that account for gender differences
Emerging Treatments and Future Directions
Precision Medicine Approaches
The future of women’s pain management lies in personalized treatment:
- Genetic testing to identify optimal medication responses
- Hormonal profiling to time treatments effectively
- Biomarker development for earlier diagnosis of pain conditions
Technology-Assisted Management
- Smartphone apps for tracking pain patterns and triggers
- Telemedicine for improved access to specialists
- Wearable devices for continuous pain and activity monitoring
Lifestyle Modifications for Chronic Pain Management
Stress Management Techniques
- Regular exercise: Low-impact activities like swimming, yoga, or walking
- Sleep hygiene: Maintaining consistent sleep schedules despite pain
- Relaxation techniques: Progressive muscle relaxation and deep breathing
Nutritional Strategies
- Anti-inflammatory diets to reduce systemic inflammation
- Adequate hydration to support overall health
- Supplements like omega-3 fatty acids and vitamin D (with medical supervision)
Frequently Asked Questions
Q: Why are women’s pain conditions often misdiagnosed or dismissed?
A: Historical medical bias, limited research on women’s pain, and cultural factors contribute to this problem. Women’s pain is more likely to be attributed to psychological causes, and many conditions predominantly affecting women have been understudied.
Q: How do hormones specifically affect chronic pain in women?
A: Estrogen and progesterone fluctuations influence pain sensitivity, inflammation levels, and neurotransmitter function. These hormonal changes can trigger pain flares, affect medication effectiveness, and influence the development of chronic pain conditions.
Q: What should I do if my doctor dismisses my chronic pain concerns?
A: Document your symptoms thoroughly, seek a second opinion, request referrals to specialists, and consider finding a healthcare provider experienced in women’s pain conditions. Don’t accept dismissive responses to persistent pain.
Q: Are there specific treatments designed for women’s chronic pain?
A: Yes, treatments are increasingly being developed with gender differences in mind, including hormone-aware medication timing, women’s health physical therapy, and trauma-informed care approaches.
Q: How can I better advocate for myself in healthcare settings?
A: Prepare detailed symptom documentation, bring specific examples of how pain affects your life, ask direct questions about treatment options, and don’t hesitate to request referrals to specialists familiar with your condition.
Taking Action: Your Next Steps
Understanding why women are more likely to experience chronic pain is the first step toward better treatment and outcomes. If you’re living with chronic pain, remember that your experience is valid and deserves proper medical attention. Work with healthcare providers who understand gender differences in pain, advocate for comprehensive evaluation, and don’t settle for dismissive responses.
The landscape of women’s pain management is evolving, with increased awareness leading to better research, treatment options, and advocacy efforts. By staying informed and actively participating in your care, you can help drive positive changes while finding the relief you deserve.
Remember: chronic pain is not something you have to endure silently. With proper understanding, advocacy, and comprehensive treatment approaches, effective pain management is possible.