Chronic pain affects over 50 million adults in the United States, making it one of the most common reasons people seek medical care. Unlike acute pain that serves as a warning signal for injury, chronic pain persists for months or even years, significantly impacting quality of life, relationships, and daily functioning. Understanding the underlying causes of chronic pain is crucial for effective treatment and management.
What Is Chronic Pain?
Chronic pain is defined as pain that persists for more than three to six months, well beyond the normal healing time for an injury or illness. Unlike acute pain, which serves a protective function by alerting us to potential harm, chronic pain often continues even after the original injury has healed.
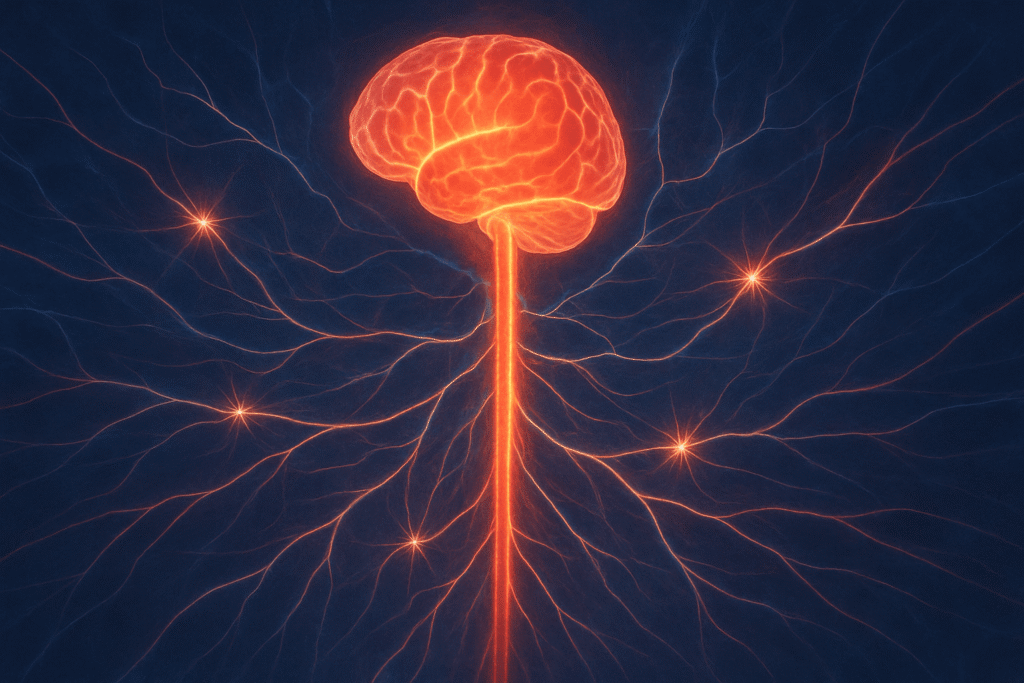
Modern pain science distinguishes between two main types of chronic pain:
- Peripheral pain: Localized pain that originates from specific tissues or organs
- Centralized pain: Pain that is processed and amplified by the brain and spinal cord, often without ongoing tissue damage
This distinction is crucial because centralized pain requires different treatment approaches than traditional peripheral pain management. Think of it like a car alarm that keeps going off even when there’s no actual threat – the alarm system itself has become hypersensitive.
The 7 Primary Causes of Chronic Pain
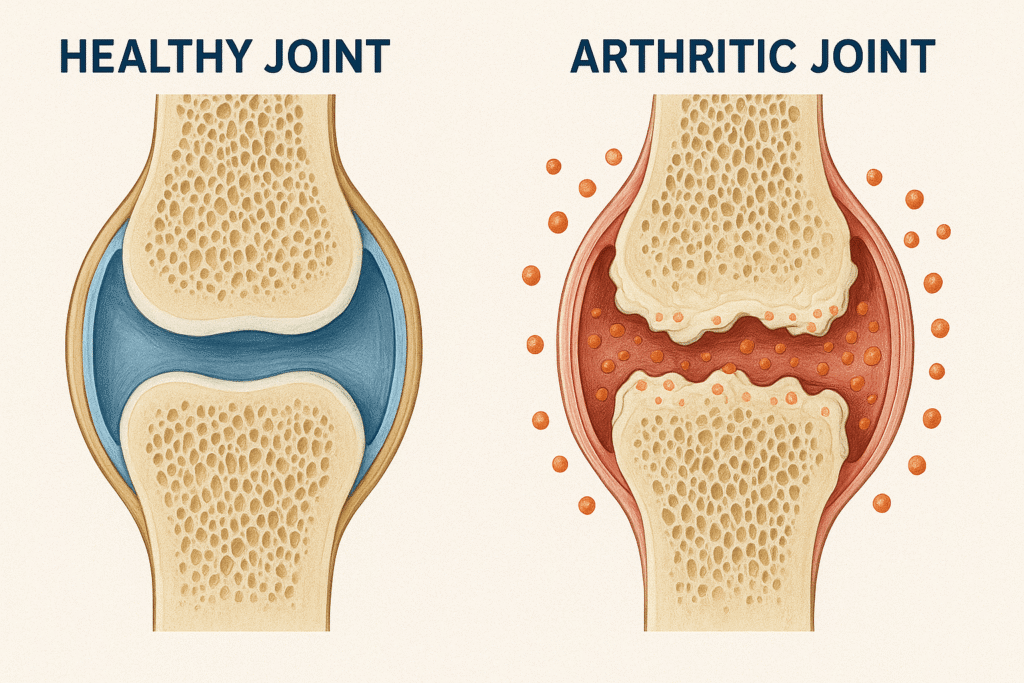
1. Arthritis and Joint Disorders
Arthritis is one of the leading causes of chronic pain, affecting over 58.5 million Americans. This umbrella term encompasses several conditions that cause joint inflammation and deterioration:
Osteoarthritis occurs when the protective cartilage that cushions joints wears down over time. This “wear and tear” arthritis commonly affects:
- Knees and hips
- Hands and fingers
- Spine
- Weight-bearing joints
Rheumatoid arthritis is an autoimmune condition where the body’s immune system attacks healthy joint tissue, causing inflammation, pain, and eventual joint damage. Unlike osteoarthritis, rheumatoid arthritis can affect multiple joints simultaneously and may also impact other organs.
The chronic pain from arthritis stems from ongoing inflammation, joint stiffness, and the body’s attempt to compensate for damaged joints, which can create additional strain on surrounding muscles and tissues.
2. Fibromyalgia and Central Sensitization
Fibromyalgia affects approximately 4 million adults in the United States and represents a classic example of centralized pain. This condition is characterized by:
- Widespread musculoskeletal pain
- Tender points throughout the body
- Fatigue and sleep disturbances
- Cognitive difficulties (“fibro fog”)
- Heightened sensitivity to touch, light, and sound
The pain in fibromyalgia occurs due to central sensitization, where the nervous system becomes hypersensitive to pain signals. The brain essentially “turns up the volume” on pain perception, making normal sensations feel painful. This neuroplasticity change explains why traditional pain medications often prove ineffective for fibromyalgia patients.
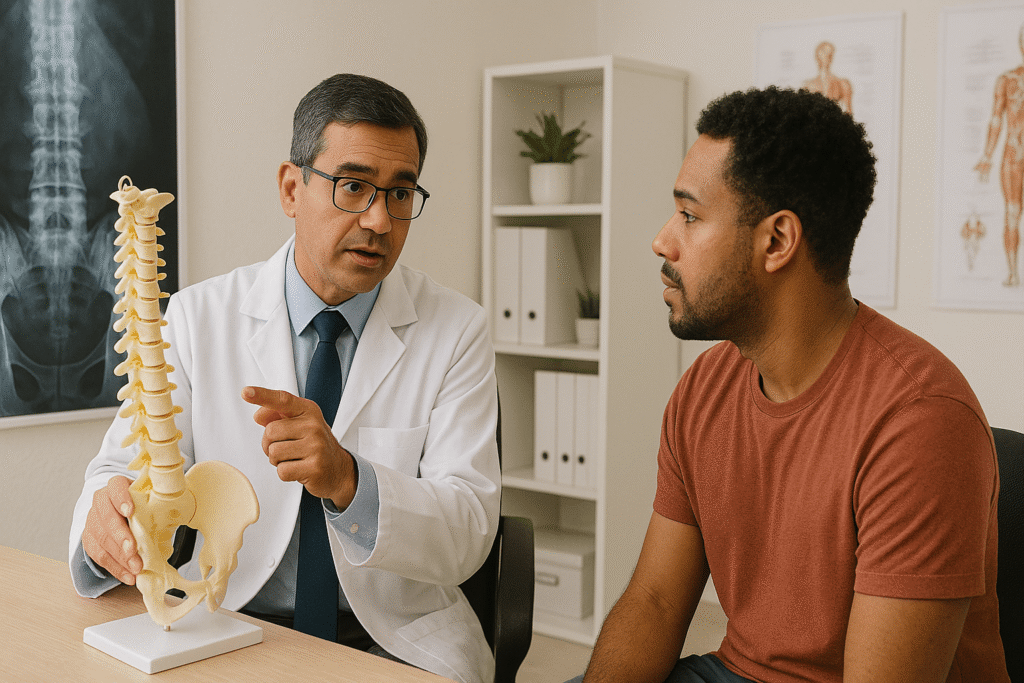
3. Chronic Back Pain and Spinal Conditions
Back pain is the leading cause of disability worldwide, with chronic back pain affecting millions of people. Several factors contribute to persistent back pain:
Structural Issues:
- Herniated or bulging discs
- Spinal stenosis (narrowing of the spinal canal)
- Spondylolisthesis (vertebrae slipping out of place)
- Degenerative disc disease
Lifestyle Factors:
- Poor posture from prolonged sitting or computer work
- Improper lifting techniques
- Weak core muscles
- Obesity placing additional stress on the spine
Age-Related Changes:
- Natural disc degeneration
- Loss of bone density
- Reduced flexibility and muscle mass
The complexity of the spine, with its intricate network of bones, discs, muscles, ligaments, and nerves, makes chronic back pain particularly challenging to treat. Often, multiple factors contribute simultaneously to ongoing pain.
4. Nerve Damage and Neuropathic Pain
Neuropathic pain results from damage or dysfunction of the nervous system itself. This type of chronic pain can be particularly challenging because it often persists even after the original cause has been addressed.
Common Causes of Nerve Damage:
- Diabetes (diabetic neuropathy)
- Chemotherapy treatments
- Shingles (postherpetic neuralgia)
- Traumatic injuries
- Autoimmune conditions
- Vitamin deficiencies
Neuropathic pain is often described as burning, shooting, or electric shock-like sensations. It may also cause numbness, tingling, or hypersensitivity to touch. The damaged nerves send abnormal pain signals to the brain, creating the perception of pain even without ongoing tissue damage.
5. Chronic Headaches and Migraines
Chronic headaches, including migraines, tension headaches, and cluster headaches, represent a significant source of ongoing pain for millions of people.
Migraine Characteristics:
- Severe, throbbing pain (often one-sided)
- Sensitivity to light, sound, and smells
- Nausea and vomiting
- Visual disturbances (aura)
- Duration of 4-72 hours
Contributing Factors:
- Genetic predisposition
- Hormonal fluctuations
- Stress and anxiety
- Sleep disturbances
- Dietary triggers
- Environmental factors
Chronic migraines (15 or more headache days per month) can significantly impact work productivity, relationships, and overall quality of life. The fear of the next migraine attack can create additional stress and anxiety, potentially triggering more episodes.
6. Inflammatory Conditions
Various inflammatory conditions can lead to chronic pain by causing ongoing tissue damage and irritation:
Endometriosis affects approximately 10% of women of reproductive age, causing chronic pelvic pain when endometrial tissue grows outside the uterus.
Inflammatory Bowel Disease (IBD), including Crohn’s disease and ulcerative colitis, can cause chronic abdominal pain, cramping, and digestive issues.
Chronic Fatigue Syndrome often includes widespread pain along with extreme fatigue that doesn’t improve with rest.
Irritable Bowel Syndrome (IBS) can cause chronic abdominal pain, bloating, and changes in bowel habits, significantly impacting daily life.
These conditions often involve complex interactions between the immune system, nervous system, and various organs, making treatment multifaceted and individualized.
7. Psychological and Lifestyle Factors
The biopsychosocial model of pain recognizes that psychological and social factors play crucial roles in chronic pain development and maintenance:
Psychological Factors:
- Depression and anxiety
- Chronic stress
- Trauma and PTSD
- Fear of movement (kinesiophobia)
- Catastrophic thinking patterns
Lifestyle Factors:
- Sedentary behavior
- Poor sleep quality
- Social isolation
- Work-related stress
- Financial concerns
Gender and Age Considerations:
Research shows that chronic pain affects women more frequently than men (21.7% vs. 19%), potentially due to hormonal factors, genetic differences, and social factors. Age also plays a significant role, with chronic pain affecting approximately 30% of adults over 65.
The Modern Approach to Chronic Pain Treatment
Understanding the complex nature of chronic pain has revolutionized treatment approaches. Modern pain management focuses on:
Multidisciplinary Care
Effective chronic pain treatment often requires a team approach involving:
- Pain specialists
- Physical therapists
- Psychologists or counselors
- Occupational therapists
- Nutritionists
- Sleep specialists
Targeted Medications
Different types of chronic pain respond to different medications:
For Centralized Pain:
- Amitriptyline (tricyclic antidepressant)
- Pregabalin and gabapentin (anticonvulsants)
- Duloxetine and venlafaxine (SNRIs)
For Inflammatory Pain:
- NSAIDs (when appropriate)
- Disease-modifying antirheumatic drugs (DMARDs)
- Biologics for autoimmune conditions
Non-Pharmacological Treatments
- Cognitive Behavioral Therapy (CBT): Helps change pain-related thoughts and behaviors
- Physical therapy: Improves strength, flexibility, and function
- Mindfulness and meditation: Reduces pain perception and stress
- Acupuncture: May help with certain types of chronic pain
- Massage therapy: Can reduce muscle tension and improve circulation
Emerging Technologies
- Neuromodulation: Spinal cord stimulators and peripheral nerve stimulators
- Regenerative medicine: Platelet-rich plasma (PRP) and stem cell therapies
- Digital health solutions: Pain tracking apps and virtual reality therapy
- Telemedicine: Improved access to specialized pain care
Prevention and Early Intervention

While not all chronic pain can be prevented, several strategies can reduce risk:
- Maintain good posture and ergonomic work environments
- Exercise regularly to strengthen muscles and maintain flexibility
- Manage stress through relaxation techniques and stress reduction
- Get adequate sleep (7-9 hours per night)
- Maintain a healthy weight to reduce joint stress
- Address acute pain promptly to prevent chronification
- Stay socially connected and maintain mental health
The Impact of Chronic Pain on Daily Life
Chronic pain extends far beyond physical discomfort, affecting:
Work and Productivity:
- Increased absenteeism
- Reduced work performance
- Career limitations
- Financial stress from medical costs
Relationships:
- Strain on family relationships
- Social isolation
- Reduced participation in activities
- Communication challenges
Mental Health:
- Increased risk of depression and anxiety
- Sleep disturbances
- Reduced self-esteem
- Feelings of helplessness
Physical Function:
- Decreased mobility and flexibility
- Muscle weakness from inactivity
- Increased risk of falls
- Secondary health problems
Moving Forward: A Comprehensive Approach
Effective chronic pain management requires understanding that pain is not just a physical sensation but a complex experience involving biological, psychological, and social factors. The shift from simply treating symptoms to addressing underlying causes and improving overall function represents a significant advancement in pain medicine.
If you’re living with chronic pain, remember that effective treatment is available. Work with healthcare providers who understand the complexity of chronic pain and are willing to develop a comprehensive, individualized treatment plan. Don’t hesitate to seek second opinions or consult with pain specialists if your current treatment isn’t providing adequate relief.
The goal isn’t necessarily to eliminate all pain but to improve function, enhance quality of life, and help you regain control over your daily activities. With the right combination of treatments and support, many people with chronic pain can lead fulfilling, productive lives.
Frequently Asked Questions
Q: How long does pain need to last to be considered chronic?
A: Pain is typically considered chronic when it persists for more than 3-6 months, well beyond the normal healing time for an injury or illness.
Q: Can chronic pain be cured?
A: While some chronic pain conditions can be cured by addressing underlying causes, many require ongoing management. The focus is often on improving function and quality of life rather than complete pain elimination.
Q: Why don’t pain medications work for all types of chronic pain?
A: Different types of chronic pain have different underlying mechanisms. Centralized pain, for example, often doesn’t respond well to traditional pain medications and may require specialized treatments like anticonvulsants or antidepressants.
Q: Is chronic pain “all in my head”?
A: Absolutely not. While psychological factors can influence pain perception, chronic pain involves real changes in the nervous system. The pain is real, regardless of whether there’s visible tissue damage.
Q: When should I see a pain specialist?
A: Consider seeing a pain specialist if your pain has lasted more than 3 months, significantly impacts your daily life, or hasn’t responded to initial treatments from your primary care provider.
Q: Can lifestyle changes really help with chronic pain?
A: Yes, lifestyle modifications including regular exercise, stress management, good sleep hygiene, and proper nutrition can significantly impact chronic pain management and overall quality of life.
Remember, chronic pain is a complex medical condition that deserves proper attention and treatment. If you’re struggling with persistent pain, don’t suffer in silence – seek help from qualified healthcare professionals who can work with you to develop an effective management strategy.